Collaborating Physician Guide: How to Legally Partner in Telemedicine sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail with casual formal language style and brimming with originality from the outset.
In the following paragraphs, we will delve into the intricacies of telemedicine collaboration, exploring its benefits, legal requirements, establishment of collaborative agreements, and risk management strategies.
Understanding Telemedicine Collaboration
Collaborating with a physician in telemedicine involves working together to provide remote healthcare services to patients using technology and virtual communication channels. This partnership allows for the exchange of medical expertise, consultations, and treatment recommendations without the need for in-person visits.Telemedicine collaboration benefits patient care by increasing access to healthcare services, especially for individuals in remote areas or those with mobility limitations.
Patients can receive timely medical advice, follow-up appointments, and specialist consultations from the comfort of their own homes. This can lead to improved health outcomes, reduced healthcare costs, and better management of chronic conditions.
Legal and Ethical Considerations
When partnering with a physician in telemedicine, it is crucial to consider the legal and ethical implications of this collaboration. Some key factors to keep in mind include:
- Compliance with state licensing regulations: Ensure that all healthcare providers involved in telemedicine are appropriately licensed in the state where the patient is located.
- Confidentiality and data security: Protect patient information by using secure communication platforms and following HIPAA guidelines to maintain privacy.
- Informed consent: Obtain consent from patients before providing telemedicine services and clearly explain the limitations of virtual consultations.
- Standard of care: Maintain the same standard of care in telemedicine as in traditional in-person visits, ensuring that patients receive high-quality medical treatment.
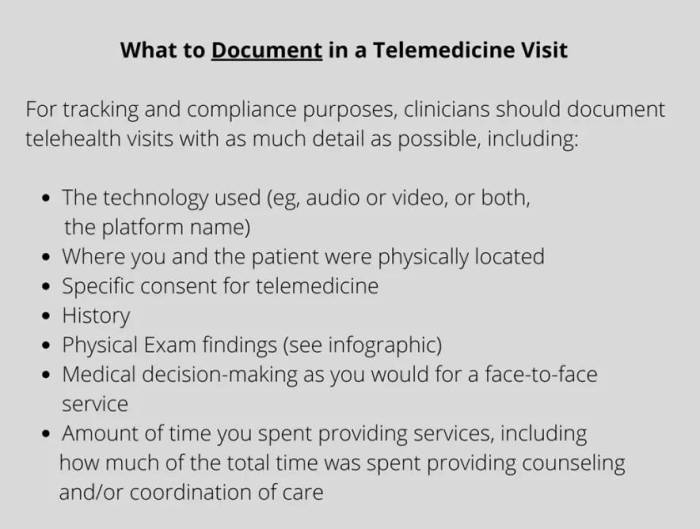
- Documentation and medical records: Keep accurate records of telemedicine consultations, including patient information, diagnoses, treatment plans, and follow-up recommendations.
Legal Requirements for Collaborating Physicians
In order to legally partner in telemedicine, physicians must adhere to specific legal requirements to ensure compliance and patient safety. Let's explore the regulations and processes involved in collaborating physicians in telemedicine.
Regulations for Collaborating Physicians in Different Regions
- In the United States, collaborating physicians must follow state-specific regulations regarding telemedicine, including licensure requirements and scope of practice limitations.
- European countries have varying regulations for collaborating physicians in telemedicine, with some countries requiring additional certifications or training.
- In Asia, regulations for collaborating physicians in telemedicine can differ significantly from country to country, impacting the ability to provide cross-border telemedicine services.
Licensing and Credentialing Process
- Physicians collaborating in telemedicine must be licensed to practice medicine in the state or country where the patient is located at the time of the consultation.
- Credentialing processes for collaborating physicians often involve verifying medical education, training, and certifications to ensure qualifications meet the standards for telemedicine practice.
- Physicians may need to obtain additional telemedicine-specific certifications or complete training programs to meet the legal requirements for providing telemedicine services.
Establishing a Collaborative Agreement
Establishing a collaborative agreement is a crucial step in forming a telemedicine partnership. This agreement Artikels the terms and conditions that both the collaborating physician and the telemedicine provider must adhere to ensure legal compliance and effective collaboration.
Key Components of a Collaborative Agreement
- Identification of Parties: Clearly specify the collaborating physician(s) and the telemedicine provider involved in the partnership.
- Scope of Services: Define the scope of medical services that the collaborating physician will provide through telemedicine.
- Roles and Responsibilities: Artikel the responsibilities of both parties, including the telemedicine provider's support and the collaborating physician's medical expertise.
- Compensation: Detail the financial arrangement, including payment structure, reimbursement processes, and any revenue sharing agreements.
- Quality Assurance: Include protocols for monitoring and evaluating the quality of telemedicine services provided by the collaborating physician.
- Compliance with Regulations: Ensure that the agreement aligns with state and federal telemedicine laws, licensing requirements, and professional standards.
Tip: It is essential to consult with legal counsel experienced in telemedicine regulations to draft a comprehensive and compliant collaborative agreement.
Ensuring Regulatory Compliance
- Stay Informed: Keep up-to-date with the evolving telemedicine regulations and adjust the agreement accordingly.
- Documentation: Maintain thorough documentation of all telemedicine activities and compliance efforts for auditing purposes.
- Training and Education: Provide ongoing training to collaborating physicians on legal requirements, best practices, and compliance protocols.
- Regular Review: Periodically review the collaborative agreement to ensure it reflects any regulatory changes and remains legally sound.
- Open Communication: Foster open communication between the telemedicine provider and collaborating physicians to address compliance issues promptly.
Risk Management Strategies
When collaborating in telemedicine, it is crucial for physicians to implement effective risk management strategies to ensure the safety of patients and the legality of the partnership.
Common Risks and Mitigation
- One common risk in telemedicine collaborations is the potential for miscommunication due to the lack of face-to-face interaction. To mitigate this risk, collaborating physicians should establish clear communication protocols and guidelines for documenting patient interactions.
- Another risk is the possibility of technical issues disrupting telemedicine sessions. Physicians can mitigate this risk by ensuring that they have reliable technology, conducting regular system checks, and having a backup plan in case of technical difficulties.
- Patient confidentiality and data security are paramount in telemedicine partnerships. Physicians should use secure communication platforms, encrypt patient data, and follow HIPAA guidelines to protect patient information from unauthorized access.
Importance of Confidentiality
Maintaining patient confidentiality and data security is not only a legal requirement but also essential for building trust with patients. By prioritizing confidentiality, collaborating physicians can uphold ethical standards and protect sensitive patient information from breaches or misuse.
Last Word

As we conclude this discussion, it becomes evident that navigating the realm of telemedicine collaboration requires a deep understanding of legal, ethical, and practical considerations. By following the guidelines Artikeld in this guide, physicians can forge successful partnerships while ensuring the highest standards of patient care and regulatory compliance.
FAQ Guide
What are the key components of a collaborative agreement in telemedicine partnerships?
The key components include roles and responsibilities of each party, duration of the agreement, dispute resolution mechanisms, and compliance with regulatory standards.
How can collaborating physicians mitigate common risks in telemedicine collaborations?
Collaborating physicians can mitigate risks by implementing robust data security measures, maintaining clear communication channels with patients, and conducting regular risk assessments.
What licensing and credentialing processes are involved for physicians collaborating in telemedicine?
Physicians need to ensure they hold valid licenses in the states where patients are located, as well as meeting credentialing requirements set by telemedicine platforms or institutions.